You’re not eating, but your belly still feels full of air. What gives?
Fasting is supposed to clear the slate, lighten the load, and maybe even shrink your waistline. But instead, your stomach feels tight, your jeans press harder, and you start to wonder if you’re doing something wrong.
You’re not. Bloating during fasting is surprisingly common, and it usually doesn’t mean you’ve “broken” your fast. It’s your digestive system adjusting to a different rhythm, plus a few habits that unintentionally make it worse.
Let’s break down what’s happening, why it happens, and how to calm it down fast.
Common Drivers of Fasting-Related Bloat
Carbonated Drinks
Sparkling water, energy drinks, and even fizzy electrolyte mixes can stretch your gut. That gas has to go somewhere, and during fasting, motility is slower, so it lingers longer. If your belly feels tight mid-morning, try switching to still water or warm tea.
Constant Gum or Sweeteners
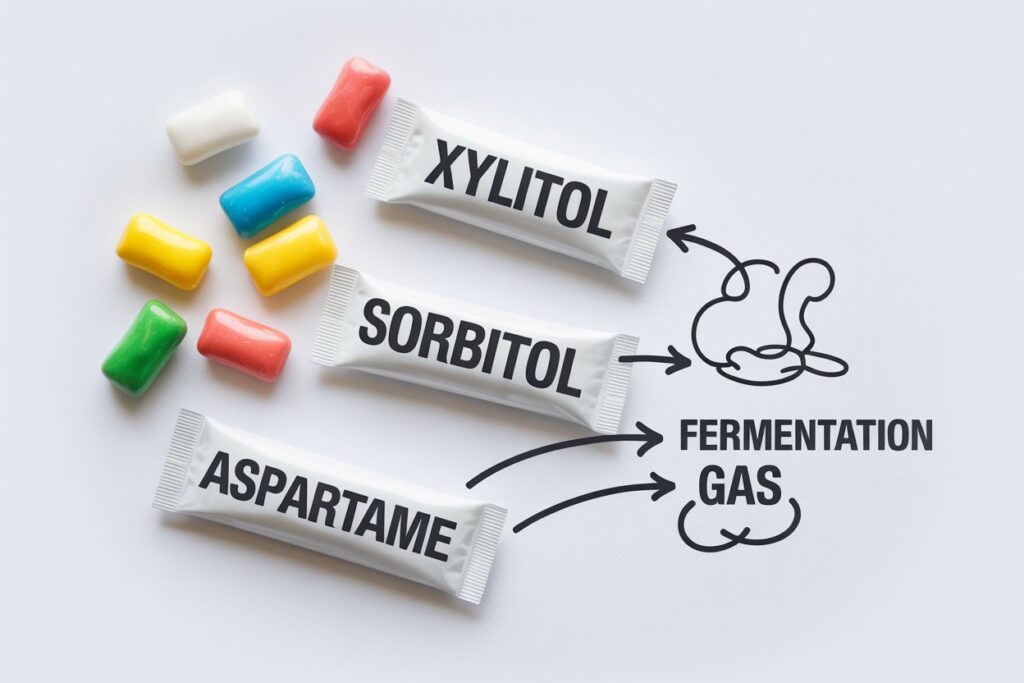
Chewing gum means swallowing more air, and sugar alcohols like xylitol or sorbitol can ferment in the colon. Artificial sweeteners may also alter gut motility and trigger mild insulin or cephalic responses. Cutting back on gum and sweet drinks for a few days often flattens things out.
Low Salt → Fluid Shifts
When you fast, glycogen stores drop. Every gram of glycogen binds about 3–4 grams of water, and when that water leaves, electrolytes like sodium and potassium shift too. Low sodium can cause fluid to move from the bloodstream into tissues, creating a “puffy yet empty” feeling. Re-adding sodium—via electrolyte tabs or a pinch of salt in water—often relieves that.
Slowed Motility
During fasting, the migrating motor complex (MMC)—your gut’s natural “housekeeping wave”—changes pace. It clears residual food and gas every 90-120 minutes in a fed state, but fasting alters those phases, which can delay clearance. A review of motility physiology confirms that fasting modifies MMC rhythm and can affect gas transit.
Coffee on an Empty Stomach
Caffeine can stimulate acid production and gut contractions. For some people, that combination feels like “wake-up energy.” For others, it means bloating, reflux, or cramping. Try lowering the dose or switching to cold brew or green tea until your gut adjusts.
Rapid Refeed
After a long fast, your gut bacteria and digestive enzymes are momentarily idle. Then you hit them with a huge plate of food. The result is just fermentation and gas. Starting with small, low-FODMAP portions allows the system to restart without overload.
FODMAP Load at First Meal
FODMAPs—fermentable carbohydrates found in garlic, onions, beans, apples, and cauliflower—are famous gas producers. If your first meal is heavy in these, you’ll feel it fast.
Stress
Even when you’re not eating, stress impacts digestion. The gut-brain axis links anxiety, hormones, and motility. Functional bloating research shows that stress increases visceral sensitivity and slows emptying.
Fasted-Window Fixes
These are small adjustments you can make without breaking your fast:
- Swap sparkling for still water. Still water eliminates swallowed air and pressure buildup.
- Limit sweeteners and gum. Give your GI tract a break from constant chewing and taste stimulation.
- Sip warm water or herbal tea. Ginger and peppermint teas can relax intestinal smooth muscle and ease bloating.
- Take short walks and use diaphragmatic breathing. Both help move gas through and activate your parasympathetic (“rest and digest”) system.
- Use electrolytes. Add sodium and potassium to maintain fluid balance and reduce “water rebound.”
- Mind motility timing. Longer fasts (48–72 hours) slow gastric emptying more than shorter fasts (~18 hours), which can increase distension risk.
If you can identify the driver and make one change—less carbonation, more salt, fewer sweeteners—bloating often subsides within a day or two.
Open-Window Strategy: Breaking the Fast Gently

When you open your eating window, reintroduce food strategically.
- Start with protein + low-FODMAP cooked vegetables. Think eggs with zucchini or chicken with spinach—easy to digest, low fermentation risk.
- Add starch and fat gradually. Once the stomach feels settled, add moderate carbs (rice, oats, potatoes) and healthy fats (olive oil, avocado).
- Save fruit for last. High-sugar fruits mixed with heavy protein or fiber can create osmotic gas.
Some other good habits to try include chewing thoroughly and eating slowly, avoiding large raw cruciferous salads on refeed days, as raw kale and cauliflower are top fermenters, and drinking plenty of fluids between meals, not during, to reduce volume pressure.
These steps mimic how clinical fasting programs structure refeeding to avoid post-fast discomfort.
Troubleshooting Persistent Bloat
If bloating continues despite tweaks, look deeper. It might be worth trying a short-term low-FODMAP trial for two to three weeks to see if fermentable carbs are the cause of your tummy troubles. Additionally, see how much fiber you’re actually ingesting. Too little can slow transit, but too much too fast can trap gas.
If your bloating comes with pain, diarrhea, constipation, or visible swelling that doesn’t resolve, talk to a clinician. Persistent distension may signal IBS, small-intestinal bacterial overgrowth, or intolerance issues.
Finally, remember that microbiota themselves produce gas. Hydrogen, methane, and carbon dioxide are natural fermentation products, and one review calls this process a normal but often misunderstood part of digestive physiology.
Use Data to Dial It In: The Fasting App by Municorn
Your gut is unique. What bloats one person might energize another. That’s why it’s important to monitor how your body responds to what you eat and when you eat. With the Fasting App, you can track:
- Hunger levels and timing
- Stool frequency and consistency
- Sweetener and carbonation intake
- Sodium/potassium use and hydration
- Fiber grams, stress levels, and exercise
- Daily bloat score (1–10)
Science-backed fasting insights, just for you.
Track your progress and get daily recommendations based on your patterns.
Over two weeks, you’ll see patterns emerge: maybe gum is the culprit, maybe low sodium, maybe it’s the timing of your first meal. The app’s graphs and notes help you make evidence-based tweaks instead of guessing.
Treat Bloating as an Opportunity to Optimize Your Fasting Schedule
Bloating while fasting is not a failure, but a chance to review your body’s feedback.
When you remove constant eating, your digestive system shifts gears. Carbonation, gum, sweeteners, low electrolytes, and fast refeeding are the usual suspects. Most cases resolve with simple fixes: still water, balanced electrolytes, slower eating, and a thoughtful refeed order.
Think of your gut as a partner in the fasting process: it needs to adjust, just like the rest of you. Give it time, move gently, and keep the data flowing.Small tweaks calm the bloat far faster than overhauling your entire fast. Try the Fasting App by Municorn today to optimize your fasting.




